Öz
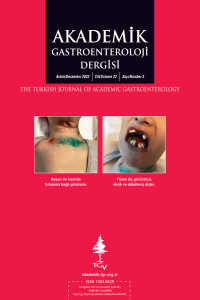
Langerhans cell histiocytosis is a rare disease with an unknown pathogenesis. It is thought that environmental factors, infections, immunological and genetic factors play a role in its etiology. Langerhans cell histiocytosis is a disorder of antigen presenting cells. It is the most common disease of the monocytic phagocytic system. Sometimes mutations (changes) develop in genes that control how dendritic cells function. These include mutations of the BRAF, MAP2K1, RAS, and ARAF genes. In the histopathology; Inflammatory cells such as T-cells, eosinophils, macrophages as well as Langerhans cells, multinucleated giant cells attract attention. The disease has a wide clinical spectrum. The clinical course varies according to the tissues and organs involved. Sometimes spontaneous recovery may occur in the clinic, as well as the disease may be progressive and fatal. Here, we will present a case diagnosed with Langerhans cell histiocytosis after many years of treatment.
Anahtar Kelimeler
Perianal lesion Langerhans cell histiocytosis Diabetes insipidus pituitary insufficiency
Kaynakça
- 1. Field M, Inston N, Muzaffar S, Cruickshank N. Perianal Langerhans cell histiocytosis. Int J Colorectal Dis 2007;22:1141-2.
- 2. Mango JCC, D’Almedia DG, Magalhaes JP, et al. Perianal Langerhans cell histiocytosis case report and review of literature. Rev Bras Coloproctol 2007;27:1.
- 3. Hamdan M, Qiao JC, Fikfak V. Adult-onset perianal Langerhans cell histiocytosis presenting as pruritus ani: a case report and review of the literatüre. J Med Case Rep 2021;15:357.
- 4. Chauffaille Mde L, Valério RM, Diniz CM, et al. Langerhans cell histiocytosis. Sao Paulo Med J 1998;116:1625-8.
- 5. Weitzman S, Egeler RM. Histiocytic disorders of children and adults: introduction to the problem, overview, historical perspective and epidemiology. In: Weitzman S, Egeler RM, editors. Histiocytic disorders of children and adults. Cambridge: Cambridge University Press 2005. p. 1-13.
- 6. Donadieu J, Egeler RM, Pritchard J. Langerhans cell histiocytosis: a clinical update. In: Weitzman S, Egeler RM, editors. Histiocytic disorders of children and adults. Cambridge: Cambridge University Press; 2005. p. 95-129.
- 7. Nakamine H, Yamakawa M, Yoshino T, Fukumoto T, Enomoto Y, Matsumura I. Langerhans cell histiocytosis and Langerhans cell sarcoma: current understanding and differential diagnosis. J Clin Exp Hematop 2016;56:109-18.
- 8. Murakami I, Matsushita M, Iwasaki T, et al. Interleukin-1 loop model for pathogenesis of Langerhans cell histiocytosis. Cell Commun Signal 2015;13:13.
- 9. Rizzo FM, Cives M, Simone V, Silvestris F. New insights into the molecular pathogenesis of Langerhans cell histiocytosis. Oncologist 2014;19:151-63.
- 10. Harmon CM, Brown N. Langerhans cell histiocytosis: a clinicopathologic review and molecular pathogenetic update. Arch Pathol Lab Med 2015;139:1211-4.
- 11. Prosch H, Grois N, Prayer D, et al. Central diabetes insipidus as presenting symptom of Langerhans cell histiocytosis. Pediatr Blood Cancer 2004;43:594-9.
- 12. Liu YH, Fan XH, Fang K. Langerhans’ cell histiocytosis with multisystem involvement in an adult. Clin Exp Dermatol 2007;32:765-8.
- 13. Bank A, Christensen C. Unusual manifestation of Langerhans’ cell histiocytosis. Acta Med Scand 1988;223:479-80.
- 14. Moroz SP, Schroeder M, Trevenen CL, Cross H. Systemic histiocytosis: an unusual cause of perianal disease in a child. J Pediatr Gastroenterol Nutr 1984;3:309-11.
- 15. Kader HA, Ruchelli E, Maller ES. Langerhans’ cell histiocytosis with stool retention caused by a perianal mass. J Pediatr Gastroenterol Nutr 1998;26:226-8.
- 16. Foster A, Epanoimeritakis M, Moorehead J. Langerhans cell histiocytosis of the perianal region. Ulster Med J 2003;72:50-1.
- 17. Gul OO, Sisman P, Cander S, et al. An unusual case of adult-onset multi-systemic Langerhans cell histiocytosis with perianal and incident thyroid involvement. Endocrinol Diabetes Metab Case Rep 2017;2017:16-0087.
- 18. Sabri M, Davie J, Orlando S, Di Lorenzo C, Ranganathan S. Gastrointestinal presentation of Langerhans cell histiocytosis in a child with perianal skin tags: a Case report. J Pediatr Gastroenterol Nutr 2004;39:564-6.
- 19. Oguzkurt P, Sarialioglu F, Ezer SS, et al. An uncommon presenting sign of Langerhans cell histiocytosis: focal perianal lesions without systemic involvement. J Pediatr Hematol Oncol 2008;30:915-6.
- 20. Akbayram S, Akgun C, Ozen S, et al. A case of Langerhans cell histiocytosis with anal fistula. Kurume Med J 2009;56:79-83.
- 21. Tinsa F, Brini I, Kharfi M, et al. Perianal presentation of Langerhans cell histiocytosis in children. Gastroenterol Clin Biol 2010;34:95-7.
- 22. Kanik A, Elacik K, Yesiloglu S, et al. An unusual presentation of Langerhans cell histiocytosis: perianal lesion. Paediatrics Today 2014;10:43-6.
- 23. Dere Y, Şahin C, Çelik SY, et al. Perianal presentation of Langerhans cell histiocytosis. Dermatol Sin 2016;34:99-101.
- 24. Waters J, Fajardo A, Holcomb B, et al. Langerhans cell histiocytosis with anorectal involvement: a rare manifestation of adult disease. Int J Colorectal Dis 2015;30:707-8.
- 25. Ronceray L, Pötschger U, Janka G, Gadner H, Minkov M; German Society for Pediatric Hematology and Oncology, Langerhans Cell Histiocytosis Study Group. Pulmonary involvement in pediatric-onset multisystem Langerhans cell histiocytosis: effect on course and outcome. J Pediatr 2012;161:129-33.e1-3.
- 26. Allen CE, Ladisch S, McClain KL. How I treat Langerhans cell histiocytosis. Blood 2015;126:26-35.
- 27. Zerbini MC, Sotto MN, Campos FP, et al. Indeterminate cell histiocytosis successfully treated with phototherapy. Autops Case Rep 2016;6:33-8.
- 28. Marchand I, Barkaoui MA, Garel C, Polak M, Donadieu J. Writing Committee. Central diabetes insipidus as the inaugural manifestation of Langerhans cell histiocytosis: natural history and medical evaluation of 26 children and adolescents. J Clin Endocrinol Metab 2011;96:E1352-60.
- 29. Shahidi-Dadras M, Saeedi M, Shakoei S, Ayatollahi A. Langerhans cell histiocytosis: an uncommon presentation, successfully treated by thalidomide. Indian J Dermatol Venereol Leprol 2011;77:587-90.
- 30. Mittal T, Davis MD, Lundell RB. Perianal Langerhans cell histiocytosis relieved by surgical excision. Br J Dermatol 2009;160:213-5.
Öz
Langerhans hücreli histiyositoz, nadir görülen ve patogenezi henüz tam olarak bilinmeyen bir hastalıktır. Etiyolojisinde çevresel etmenler, enfeksiyonlar, immünolojik ve genetik etkenlerin rol oynadığı düşünülmektedir. Langerhans hücreli histiyositoz, antijen sunan hücrelerin bir bozukluğudur. Monositer fagositer sistemin en sık görülen hastalığıdır. Bazen dendritik hücrelerin nasıl çalıştığını kontrol eden genlerde mutasyonlar (değişiklikler) gelişir. Bunlar BRAF, MAP2K1, RAS ve ARAF genlerinin mutasyonlarını içerir. Histopatolojisinde; Langerhans hücreleri kadar T-hücreleri, eozinofil, makrofajlar gibi inflamasyon hücreleri yanında, çok çekirdekli dev hücreler dikkati çeker. Hastalığın klinik olarak geniş bir yelpazesi vardır. Tutulan doku ve organlara göre klinik seyir çeşitlilik gösterir. Klinikte bazen kendiliğinden iyileşme olabildiği gibi, hastalık ilerleyici ve ölümcül de olabilir. Burada uzun yıllar tedavi sonunda Langerhans hücreli histiyositoz tanısı alan bir vakayı sunacağız.
Anahtar Kelimeler
Perianal lezyon Langerhans hücreli histiyositoz Diabetes insipidus hipofizer yetmezlik
Kaynakça
- 1. Field M, Inston N, Muzaffar S, Cruickshank N. Perianal Langerhans cell histiocytosis. Int J Colorectal Dis 2007;22:1141-2.
- 2. Mango JCC, D’Almedia DG, Magalhaes JP, et al. Perianal Langerhans cell histiocytosis case report and review of literature. Rev Bras Coloproctol 2007;27:1.
- 3. Hamdan M, Qiao JC, Fikfak V. Adult-onset perianal Langerhans cell histiocytosis presenting as pruritus ani: a case report and review of the literatüre. J Med Case Rep 2021;15:357.
- 4. Chauffaille Mde L, Valério RM, Diniz CM, et al. Langerhans cell histiocytosis. Sao Paulo Med J 1998;116:1625-8.
- 5. Weitzman S, Egeler RM. Histiocytic disorders of children and adults: introduction to the problem, overview, historical perspective and epidemiology. In: Weitzman S, Egeler RM, editors. Histiocytic disorders of children and adults. Cambridge: Cambridge University Press 2005. p. 1-13.
- 6. Donadieu J, Egeler RM, Pritchard J. Langerhans cell histiocytosis: a clinical update. In: Weitzman S, Egeler RM, editors. Histiocytic disorders of children and adults. Cambridge: Cambridge University Press; 2005. p. 95-129.
- 7. Nakamine H, Yamakawa M, Yoshino T, Fukumoto T, Enomoto Y, Matsumura I. Langerhans cell histiocytosis and Langerhans cell sarcoma: current understanding and differential diagnosis. J Clin Exp Hematop 2016;56:109-18.
- 8. Murakami I, Matsushita M, Iwasaki T, et al. Interleukin-1 loop model for pathogenesis of Langerhans cell histiocytosis. Cell Commun Signal 2015;13:13.
- 9. Rizzo FM, Cives M, Simone V, Silvestris F. New insights into the molecular pathogenesis of Langerhans cell histiocytosis. Oncologist 2014;19:151-63.
- 10. Harmon CM, Brown N. Langerhans cell histiocytosis: a clinicopathologic review and molecular pathogenetic update. Arch Pathol Lab Med 2015;139:1211-4.
- 11. Prosch H, Grois N, Prayer D, et al. Central diabetes insipidus as presenting symptom of Langerhans cell histiocytosis. Pediatr Blood Cancer 2004;43:594-9.
- 12. Liu YH, Fan XH, Fang K. Langerhans’ cell histiocytosis with multisystem involvement in an adult. Clin Exp Dermatol 2007;32:765-8.
- 13. Bank A, Christensen C. Unusual manifestation of Langerhans’ cell histiocytosis. Acta Med Scand 1988;223:479-80.
- 14. Moroz SP, Schroeder M, Trevenen CL, Cross H. Systemic histiocytosis: an unusual cause of perianal disease in a child. J Pediatr Gastroenterol Nutr 1984;3:309-11.
- 15. Kader HA, Ruchelli E, Maller ES. Langerhans’ cell histiocytosis with stool retention caused by a perianal mass. J Pediatr Gastroenterol Nutr 1998;26:226-8.
- 16. Foster A, Epanoimeritakis M, Moorehead J. Langerhans cell histiocytosis of the perianal region. Ulster Med J 2003;72:50-1.
- 17. Gul OO, Sisman P, Cander S, et al. An unusual case of adult-onset multi-systemic Langerhans cell histiocytosis with perianal and incident thyroid involvement. Endocrinol Diabetes Metab Case Rep 2017;2017:16-0087.
- 18. Sabri M, Davie J, Orlando S, Di Lorenzo C, Ranganathan S. Gastrointestinal presentation of Langerhans cell histiocytosis in a child with perianal skin tags: a Case report. J Pediatr Gastroenterol Nutr 2004;39:564-6.
- 19. Oguzkurt P, Sarialioglu F, Ezer SS, et al. An uncommon presenting sign of Langerhans cell histiocytosis: focal perianal lesions without systemic involvement. J Pediatr Hematol Oncol 2008;30:915-6.
- 20. Akbayram S, Akgun C, Ozen S, et al. A case of Langerhans cell histiocytosis with anal fistula. Kurume Med J 2009;56:79-83.
- 21. Tinsa F, Brini I, Kharfi M, et al. Perianal presentation of Langerhans cell histiocytosis in children. Gastroenterol Clin Biol 2010;34:95-7.
- 22. Kanik A, Elacik K, Yesiloglu S, et al. An unusual presentation of Langerhans cell histiocytosis: perianal lesion. Paediatrics Today 2014;10:43-6.
- 23. Dere Y, Şahin C, Çelik SY, et al. Perianal presentation of Langerhans cell histiocytosis. Dermatol Sin 2016;34:99-101.
- 24. Waters J, Fajardo A, Holcomb B, et al. Langerhans cell histiocytosis with anorectal involvement: a rare manifestation of adult disease. Int J Colorectal Dis 2015;30:707-8.
- 25. Ronceray L, Pötschger U, Janka G, Gadner H, Minkov M; German Society for Pediatric Hematology and Oncology, Langerhans Cell Histiocytosis Study Group. Pulmonary involvement in pediatric-onset multisystem Langerhans cell histiocytosis: effect on course and outcome. J Pediatr 2012;161:129-33.e1-3.
- 26. Allen CE, Ladisch S, McClain KL. How I treat Langerhans cell histiocytosis. Blood 2015;126:26-35.
- 27. Zerbini MC, Sotto MN, Campos FP, et al. Indeterminate cell histiocytosis successfully treated with phototherapy. Autops Case Rep 2016;6:33-8.
- 28. Marchand I, Barkaoui MA, Garel C, Polak M, Donadieu J. Writing Committee. Central diabetes insipidus as the inaugural manifestation of Langerhans cell histiocytosis: natural history and medical evaluation of 26 children and adolescents. J Clin Endocrinol Metab 2011;96:E1352-60.
- 29. Shahidi-Dadras M, Saeedi M, Shakoei S, Ayatollahi A. Langerhans cell histiocytosis: an uncommon presentation, successfully treated by thalidomide. Indian J Dermatol Venereol Leprol 2011;77:587-90.
- 30. Mittal T, Davis MD, Lundell RB. Perianal Langerhans cell histiocytosis relieved by surgical excision. Br J Dermatol 2009;160:213-5.
Ayrıntılar
| Birincil Dil | Türkçe |
|---|---|
| Konular | Gastroenteroloji ve Hepatoloji |
| Bölüm | Makaleler |
| Yazarlar | |
| Yayımlanma Tarihi | 22 Aralık 2023 |
| Yayımlandığı Sayı | Yıl 2023 Cilt: 22 Sayı: 3 |
test-5